5 Powerful Facts About Metabolic Syndrome and Endometrial Cancer Risk You Can’t Ignore
Explore how metabolic syndrome and endometrial cancer risk are deeply connected in ways most people overlook. This concise, research-backed teaser highlights key dangers, early warning insights, and crucial steps every woman should know.
Metabolic syndrome and endometrial cancer risk have become a major concern in women’s health research. Recent clinical studies suggest that women with metabolic syndrome (MetS) face a 30–50% higher risk of developing endometrial cancer compared to women without MetS.
This article explains what metabolic syndrome is, how it contributes to cancer development, and what the findings mean for prevention and public health.
- Metabolic syndrome significantly increases endometrial cancer risk.
- Central obesity and insulin resistance are the strongest contributing factors.
- Early lifestyle management can reduce both metabolic and cancer risks.
Quick Context
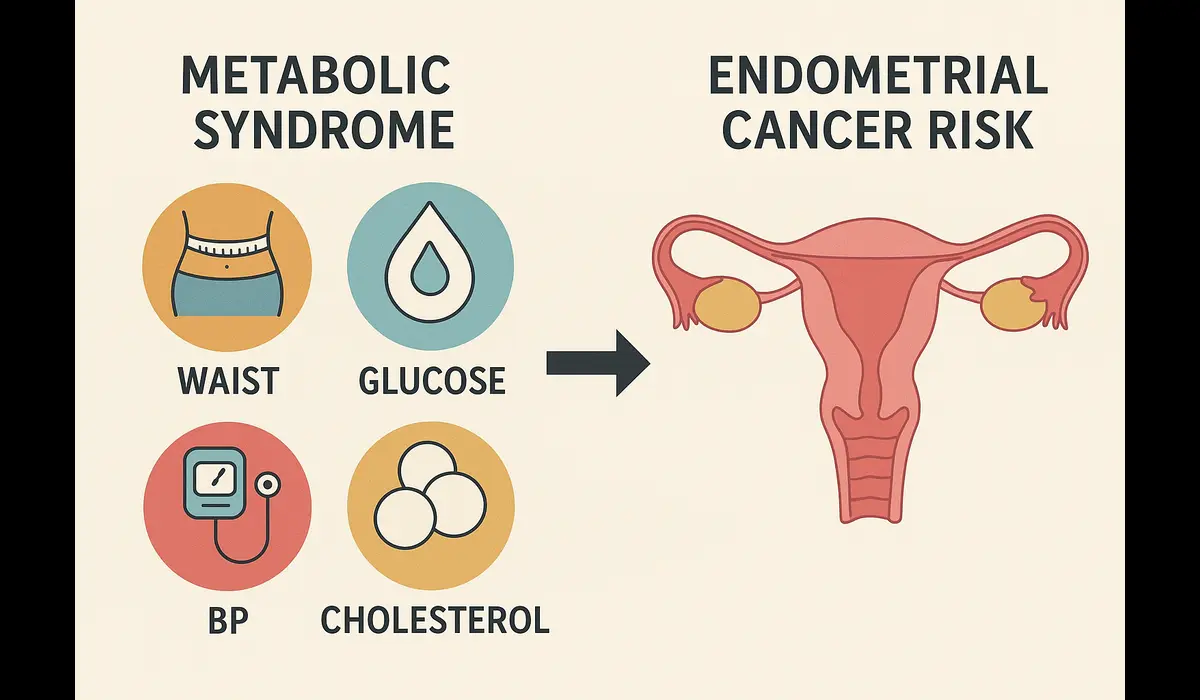
Thisis a combination of interconnected health conditions — abdominal obesity, high blood sugar, high blood pressure, and abnormal cholesterol levels — that raise the risk of cardiovascular diseases and type 2 diabetes.
Recent medical evidence shows that these same metabolic disturbances also play a critical role in increasing the risk of endometrial cancer, a malignancy of the uterine lining.

$500 Walmart Gift Card$500 Walmart Gift Card
Some users qualify for a $500 Walmart gift card. You can check if you qualify.
Latest Study Findings
The latest epidemiological studies on metabolic syndrome and endometrial cancer risk reveal:
- Women with full metabolic syndrome are 1.3–1.5 times more likely to develop endometrial carcinoma.
- The risk increases proportionally with the number of MetS components present (e.g., obesity + hyperglycemia + hypertension).
- Central obesity and insulin resistance show the strongest correlation among all components.
- The association persists even after adjusting for overall BMI, meaning metabolic dysfunction is a risk factor independent of body weight.
These findings underline that metabolic syndrome is not just a cardiovascular issue — it’s an oncologic risk multiplier for women.
Key Facts
1. Role of Obesity and Insulin Resistance
Excess abdominal fat increases estrogen production and inflammation, both of which stimulate endometrial cell proliferation.
Insulin resistance and high insulin levels also act as growth promoters for endometrial tissue, creating an environment where cancer can thrive.
2. Chronic Inflammation
Metabolic syndrome is associated with elevated inflammatory markers such as CRP and IL-6. These inflammatory processes can damage DNA and promote abnormal cell growth in the uterine lining.
3. Hormonal Imbalance
Women with MetS often have higher circulating estrogen and lower sex hormone–binding globulin (SHBG) levels. This hormonal imbalance increases the lifetime exposure of the endometrium to estrogen — a known cancer driver.
4. Dyslipidemia and Hypertension
High triglycerides and blood pressure alter endothelial function, leading to metabolic stress and oxidative damage in reproductive tissues.
Why It Matters
1. Growing Global Prevalence
With over 25% of adult women worldwide now meeting the criteria for metabolic syndrome, the connection to endometrial cancer represents a growing public health challenge.
2. Preventable Risk Factor
Unlike genetic predisposition, metabolic syndrome is largely preventable through lifestyle and early intervention. Addressing it early could reduce both metabolic and cancer burdens.
3. Clinical Screening Opportunity
Gynecologists and primary care physicians can use metabolic indicators as early warning signals for endometrial cancer risk. This allows for proactive monitoring and preventive care.
Comparative Analysis
| Risk Factor | Strength of Association | Preventability |
|---|---|---|
| Obesity | Strong | High |
| Metabolic Syndrome | Strong | High |
| Diabetes | Moderate | Moderate |
| Estrogen Therapy | Strong | Moderate |
| Family History | Moderate | Low |
This table shows that metabolic syndrome and obesity rank among the most significant modifiable risk factors for endometrial cancer.
Evidence & Expert Opinion
Medical researchers suggest that metabolic syndrome creates a pro-inflammatory, estrogen-dominant, insulin-driven environment that supports cancer development.
Experts emphasize:
- Women with both MetS and obesity face the highest risk levels.
- Even normal-weight women with insulin resistance or elevated triglycerides can have a heightened cancer risk.
- Interventions targeting weight reduction, insulin sensitivity, and blood pressure control show potential in risk reduction.
While more longitudinal studies are needed, current findings strongly support including metabolic health management in women’s cancer prevention strategies.
Practical Takeaways
- Monitor Metabolic Health:
Regularly check waist circumference, blood pressure, fasting glucose, and lipid profile. - Adopt a Balanced Diet:
Choose a diet rich in vegetables, lean protein, and omega-3 fats. Limit refined carbs and sugary drinks to improve insulin sensitivity. - Increase Physical Activity:
Engage in at least 150 minutes of moderate exercise weekly to maintain healthy weight and hormone balance. - Control Blood Sugar and Blood Pressure:
Work with healthcare professionals to keep metabolic markers within optimal ranges. - Get Regular Screenings:
If you have metabolic syndrome or PCOS, discuss periodic endometrial screening with your gynecologist.

$750 Cash App Gift Card$750 Cash App Gift Card
Some users qualify for a $750 Cash App gift card. You can check if you qualify.
FAQs
Q1: What does the study on metabolic syndrome and endometrial cancer risk show?
It shows that women with metabolic syndrome are significantly more likely to develop endometrial cancer due to insulin resistance, obesity, and inflammation.
Q2: Can a healthy-weight woman have metabolic syndrome?
Yes. Even normal-weight women with poor metabolic profiles — high blood sugar, triglycerides, or blood pressure — may have metabolic syndrome and elevated cancer risk.
Q3: Which factor in metabolic syndrome is most dangerous?
Central (abdominal) obesity and insulin resistance have the strongest link to endometrial cancer.
Q4: Can lifestyle changes reverse this risk?
Yes. Weight loss, improved diet, and exercise can normalize metabolic parameters and potentially reduce cancer risk.
Q5: Is the risk permanent once diagnosed with MetS?
No. Early intervention and sustained lifestyle modification can reverse metabolic syndrome and lower overall health risks.
Key Takeaways
- Metabolic syndrome and endometrial cancer risk are closely connected through obesity, insulin resistance, and inflammation.
- The relationship holds even in non-obese women.
- Preventive measures such as diet, exercise, and early detection can lower risk.
- Managing metabolic syndrome benefits both cardiovascular and reproductive health.
Conclusion
The growing evidence linking metabolic syndrome and endometrial cancer risk highlights a crucial intersection between metabolic health and oncology. By controlling blood sugar, reducing waist circumference, and improving insulin sensitivity, women can substantially lower their chances of developing endometrial cancer.
Metabolic health is not just about avoiding diabetes — it’s about protecting your long-term hormonal and reproductive well-being.





